

NDVH (Non-Descent Vaginal Hysterectomy) is a safe and scar-free way to remove the uterus.
A retrospective research was conducted at the Department of Obstetrics and Gynecology of Shree Dharmasthala Manjunatheshwara (SDM) College of Medical Sciences and Hospital in Dharwad, India, from May 2014 to May 2017. Hysterectomies were attempted vaginally in women with benign illnesses and large uteri. Age, parity, uterine size, blood loss, operation time, number of fibroids, further surgical problems, and intraoperative and postoperative complications were all recorded.
If the uterus is not prolapsed, this sort of vaginal hysterectomy can be performed. Because the uterus is removed through the body's natural orifice/opening, there are no visible scars (vagina). Because of this, NDVH is sometimes referred to as a scarless hysterectomy or scarless surgery.
Common Reasons for a Non-Descent Vaginal Hysterectomy :
Uterine Fibroids
Uterine fibroids are non-cancerous growths in the uterine wall. The fibroid tumors may grow very large and put pressure on other pelvic organs. Women who have uterine fibroids may experience heavy bleeding or severe pelvic pain in some cases.
Gynecological Cancer
A hysterectomy may be the best course of treatment in some cases of gynecological cancer or precancer. This includes uterine cancer, ovarian cancer, cervical cancer, and cancer of the uterine lining. Other treatments for these conditions include radiation and chemotherapy and your doctor will determine which is best for you based on how advanced the disease is.
Uterine Prolapse
Uterine prolapse is a condition in which the uterus is displaced and slips into the vagina. Prolapse is often found in women who have given birth multiple times and can also be a problem for obese women and postmenopausal women. The condition can cause urinary and bowel issues as well as pelvic pain or pressure.
Abnormal Bleeding
Heavy or prolonged bleeding caused by infection, cancer, hormone imbalance, or fibroids can be potentially dangerous. When other treatment options fail, a hysterectomy may be suggested.
Endometriosis
Endometriosis is a condition in which the tissue that lines the uterus grows outside of the uterus (in the pelvic cavity, on ovaries and fallopian tubes, and the outer surface of the uterus). The tissue growth causes bleeding between menstrual periods and pain that can get very intense and interfere with daily life. This chronic condition does not have a cure and in severe cases, a hysterectomy may be recommended.
Endometrial Hyperplasia
Endometrial hyperplasia refers to the over-thickening of the uterine lining. It is often caused by the presence of estrogen without progesterone for prolonged periods of time, which can happen during times when hormone levels are changing, like during perimenopause.
Adenomyosis
Adenomyosis is a condition similar to endometriosis in that it involves the growth of uterine lining where it should not grow. However, unlike endometriosis, the tissue grows inside the walls of the uterus where it does not belong which can cause bleeding and pain.
Severe Pelvic Inflammatory Disease (PID)
Pelvic inflammatory disease (PID) is a bacterial infection in the pelvic cavity that can cause severe pelvic pain. When caught early, PID can be treated with antibiotics. However, if the infection is left untreated and spreads, it can damage the uterus.
The procedure is normally done under a general anaesthesia, but several anaesthetic procedures might be used. The procedure normally takes 45 minutes.
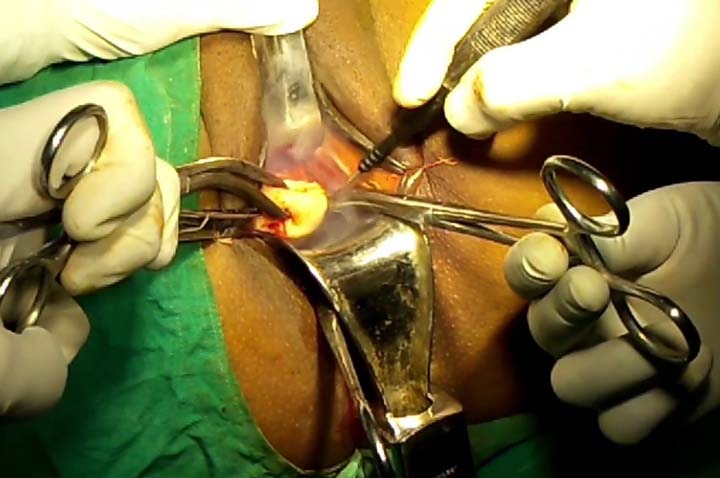
Your vagina will be examined by your gynaecologist. They will make a cut at the top of your vaginal wall around your cervix to remove your womb and cervix.
To prevent the chance of recurrent prolapse, they will usually sew the support ligaments of your womb to the top of your vagina and may implant a pack (similar to a large tampon) in your vagina.
A hysterectomy is regarded as a relatively risk-free treatment. However, as with any major surgery, there are hazards involved. An allergic reaction to the anaesthesia is possible in certain people. There's also a chance of a lot of bleeding and infection near the incision.
Other risks include injury to surrounding tissues or organs, including the:
bladder
intestines
blood vessels

